Understanding Hemorrhoids
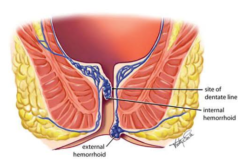
Hemorrhoids are swollen and inflamed veins in the lower rectum and anus, similar to varicose veins. They can develop inside the rectum (internal hemorrhoids) or under the skin around the anus (external hemorrhoids). Hemorrhoids are common, especially among adults over 50, but they can affect people of all ages. While often uncomfortable and sometimes painful, hemorrhoids are generally not serious and can be treated with various methods, including surgery in more severe cases.
Recognizing Hemorrhoid Symptoms
Pain and Discomfort
Pain and discomfort are the most noticeable symptoms of hemorrhoids, particularly external hemorrhoids. The discomfort can range from mild irritation to significant pain, especially during bowel movements. Sitting for long periods can also exacerbate the pain, making daily activities challenging for those affected.
Itching and Irritation
Hemorrhoids often cause itching around the anus due to the irritation of the skin in this area. The itching can be persistent and may worsen after a bowel movement. This irritation is caused by the swelling and inflammation of the veins, which can lead to further discomfort if not treated properly.
Bleeding
Bleeding during bowel movements is a common symptom of hemorrhoids. You may notice bright red blood on the toilet paper, in the toilet bowl, or on the surface of your stool. While bleeding is usually minor, any persistent or significant bleeding should be evaluated by a healthcare provider to rule out more serious conditions.
Swelling and Lumps
External hemorrhoids can cause noticeable swelling around the anus. In some cases, a painful lump may form due to a blood clot in the hemorrhoid, known as a thrombosed hemorrhoid. This lump can cause severe pain and discomfort, and in some instances, may require medical intervention.
Prolapse
Internal hemorrhoids can sometimes prolapse, meaning they push through the anal opening. Prolapsed hemorrhoids can be painful and may cause a feeling of fullness or discomfort in the rectum. They can often be pushed back inside, but in more severe cases, medical treatment may be necessary to manage the condition.
When Is Surgery Necessary for Hemorrhoids?
Non-Surgical Treatment Options
Before considering surgery, doctors typically recommend non-surgical treatments for hemorrhoids. These include lifestyle changes, such as increasing fiber intake to prevent constipation, drinking plenty of water, and using over-the-counter creams or suppositories to relieve symptoms. Sitz baths, which involve soaking the affected area in warm water, can also help reduce pain and swelling. For mild to moderate hemorrhoids, these treatments are often effective in managing symptoms.
Indications for Surgery
Surgery may be necessary when hemorrhoids cause severe pain, persistent bleeding, or prolapse that cannot be managed with non-surgical treatments. Hemorrhoid surgery is typically recommended when:
- Non-surgical treatments have failed to relieve symptoms.
- The hemorrhoids are large and cause significant discomfort.
- There is persistent or heavy bleeding that leads to anemia.
- A thrombosed hemorrhoid causes severe pain and does not improve with conservative treatment.
- Prolapsed hemorrhoids cannot be repositioned or cause ongoing symptoms.
Types of Hemorrhoid Surgery
Hemorrhoidectomy
A hemorrhoidectomy is the most common surgical procedure for removing hemorrhoids. This surgery involves cutting out the hemorrhoid tissue and is usually performed under general anesthesia. Hemorrhoidectomy is highly effective for treating severe or recurrent hemorrhoids, but it requires a recovery period of several weeks. During recovery, patients may experience pain and discomfort, which can be managed with pain relievers and sitz baths.
Stapled Hemorrhoidopexy
Stapled hemorrhoidopexy, also known as stapling, is a less invasive surgical option that is often used for prolapsed hemorrhoids. This procedure involves using a stapling device to remove part of the hemorrhoid and reposition the remaining tissue back inside the rectum. Stapling generally results in less pain and a quicker recovery compared to hemorrhoidectomy, but it may have a higher risk of recurrence.
Rubber Band Ligation
Rubber band ligation is a minimally invasive procedure where a small band is placed around the base of an internal hemorrhoid to cut off its blood supply. The hemorrhoid shrinks and eventually falls off within a week or two. This procedure is usually performed in a doctor’s office and does not require anesthesia. While effective for small to medium-sized hemorrhoids, rubber band ligation may not be suitable for larger or more severe hemorrhoids.
Sclerotherapy
Sclerotherapy involves injecting a chemical solution into the hemorrhoid to shrink it. This procedure is less commonly used but can be effective for treating small internal hemorrhoids. Sclerotherapy is usually done in an outpatient setting and causes minimal discomfort. However, it may require multiple sessions to achieve the desired results.
Recovery and Post-Surgery Care
Managing Pain and Discomfort
After hemorrhoid surgery, managing pain and discomfort is a key part of the recovery process. Pain relievers are often prescribed to help manage the pain during the first few days after surgery. Sitz baths, which involve soaking the area in warm water several times a day, can also provide relief and promote healing. It’s important to follow your doctor’s instructions regarding activity levels, as you may need to avoid strenuous activities for a few weeks.
Preventing Recurrence
Preventing the recurrence of hemorrhoids after surgery involves making certain lifestyle changes. Increasing fiber intake and staying hydrated can help prevent constipation, which is a major cause of hemorrhoids. Regular exercise and avoiding prolonged sitting can also help reduce the risk of hemorrhoids returning. Maintaining a healthy weight is important as well, as excess weight can increase pressure on the veins in the lower rectum and anus.
Follow-Up Care
Regular follow-up visits with your healthcare provider are important after hemorrhoid surgery to monitor your recovery and ensure that the hemorrhoids do not return. During these visits, your doctor may recommend additional treatments or lifestyle changes to help prevent future problems. If you experience any unusual symptoms or complications after surgery, such as excessive bleeding, fever, or severe pain, it’s important to contact your doctor immediately.
Conclusion
Summary of Key Points
Hemorrhoids are a common condition that can cause significant discomfort, pain, and bleeding. Recognizing the symptoms early and seeking appropriate treatment can prevent complications. While many cases of hemorrhoids can be managed with lifestyle changes and non-surgical treatments, surgery may be necessary for severe or persistent cases. Understanding the different surgical options, from hemorrhoidectomy to minimally invasive procedures like rubber band ligation, can help patients make informed decisions about their care.
Encouragement to Seek Help
If you experience symptoms of hemorrhoids, such as pain, bleeding, or prolapse, don’t hesitate to consult a healthcare provider. Early intervention can prevent the condition from worsening and improve your quality of life. If surgery is necessary, your doctor can help you choose the best option based on your specific needs and symptoms.
