What is Hepatitis C?
Hepatitis C is a viral infection that affects the liver and is caused by the Hepatitis C virus (HCV). It spreads primarily through contact with infected blood and can lead to both short-term and long-term health complications. Over time, if left untreated, Hepatitis C can cause severe liver damage, including cirrhosis, liver failure, and liver cancer.
Hepatitis C infections are classified into two categories: acute and chronic. Acute Hepatitis C occurs within the first six months after exposure to the virus. Some individuals may clear the virus naturally during this phase. Still, for most, the infection progresses to chronic Hepatitis C. Chronic infections persist for years, often without noticeable symptoms, gradually damaging the liver over time.
How Does Hepatitis C Spread?
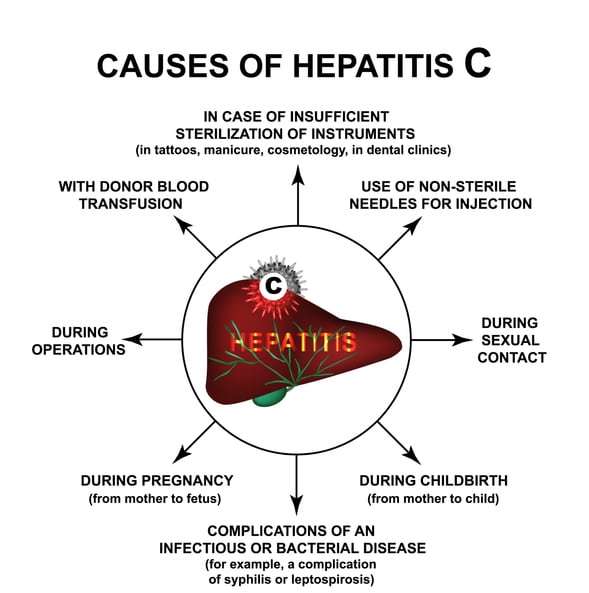
Hepatitis C spreads through blood-to-blood contact. The most common transmission methods include:
- Sharing needles or syringes during drug use.
- Receiving a blood transfusion or organ transplant before 1992, when more rigorous screening of the blood supply began.
- Accidental needle-stick injuries in healthcare settings.
- Using non-sterile equipment for tattoos or piercings.
Hepatitis C is less commonly spread through sexual contact or from an infected mother to her baby during childbirth. It is not transmitted through casual contact like hugging, sharing food, or sneezing.
Common Symptoms of Hepatitis C
Hepatitis C is often called a silent infection because many people do not experience symptoms until significant liver damage has occurred. However, some individuals may develop early symptoms during the acute phase of infection.
Symptoms of acute Hepatitis C include fatigue, fever, nausea, abdominal pain, and jaundice. Dark-colored urine and pale stools may also appear. These symptoms typically occur within two weeks to six months after exposure to the virus. They may resolve on their own in some cases.
Chronic Hepatitis C often remains asymptomatic for years but can eventually lead to noticeable signs of liver damage. These symptoms may include persistent fatigue, abdominal or leg swelling, and easy bruising or bleeding. As liver function declines, complications such as cirrhosis or liver failure can develop, leading to more severe symptoms like confusion, significant weight loss, and yellowing of the skin and eyes.
How is Hepatitis C Diagnosed?
Diagnosing Hepatitis C involves blood tests to detect the presence of the virus. The initial screening test looks for HCV antibodies, which indicate whether a person has been exposed to the virus. If antibodies are detected, a follow-up test measures the viral RNA to confirm an active infection.
Early testing is crucial for preventing complications and reducing the risk of transmission. Those at higher risk, such as individuals who use intravenous drugs, healthcare workers with accidental exposure, or people with a history of unprotected sex, should undergo regular screening. The Centers for Disease Control and Prevention (CDC) also recommends one-time testing for all adults and pregnant individuals during each pregnancy.
Treatment Options for Hepatitis C
The treatment landscape for Hepatitis C has improved dramatically in recent years. Direct-acting antivirals (DAAs) are now the standard treatment and have transformed how the infection is managed. These medications work by targeting specific steps in the virus’s replication process, effectively stopping it from multiplying and allowing the body to eliminate it.
DAAs are taken orally, typically once a day, for 8 to 12 weeks. Treatment is highly effective, with cure rates exceeding 95 percent for most patients. Unlike older treatments, DAAs are well-tolerated, with fewer side effects such as fatigue, nausea, or headache. This makes them accessible to a broader range of patients, including those with underlying conditions.
For individuals with advanced liver damage or cirrhosis, treatment plans may need to be tailored to account for their liver health. While DAAs can still cure the virus in these cases, managing liver function during and after treatment is crucial to preventing further complications.
Successful treatment eliminates the virus and significantly reduces the risk of liver-related illnesses. Patients are encouraged to adhere strictly to their prescribed treatment regimen to maximize their chances of achieving a cure.
Lifestyle Changes During and After Treatment
While antiviral therapy is highly effective, maintaining a healthy lifestyle can further support liver health and improve treatment outcomes. Eating a balanced diet, staying hydrated, and avoiding alcohol are all essential for reducing strain on the liver. Alcohol consumption can accelerate liver damage, making it vital to abstain completely during treatment.
Regular exercise can also promote overall health and help manage symptoms like fatigue. Additionally, individuals with Hepatitis C should avoid taking medications that may be harsh on the liver without consulting their healthcare provider.
Preventing the Spread of Hepatitis C
Hepatitis C is preventable through simple but effective measures to reduce the risk of exposure. Avoiding the sharing of needles, syringes, or other drug paraphernalia is one of the most critical steps. People who
