Celiac disease is a serious autoimmune disorder that occurs in genetically predisposed individuals where the ingestion of gluten leads to damage in the small intestine. Gluten, a protein found in wheat, barley, and rye, triggers an immune response that attacks the lining of the small intestine, leading to malabsorption of nutrients and a variety of gastrointestinal and systemic symptoms. Understanding the complexities of celiac disease, from its causes to effective management strategies, is crucial for those affected. This document aims to provide a comprehensive overview of celiac disease, encompassing its pathophysiology, diagnosis, and practical approaches to living a gluten-free life.
Symptoms of Celiac Disease
Celiac disease can affect different people in different ways, and symptoms can vary greatly in both type and severity. Some common symptoms include:
- Digestive Issues: Diarrhea, constipation, abdominal pain, bloating, gas, and indigestion are common.
- Weight Loss and Fatigue: Malabsorption of nutrients can lead to unintentional weight loss and persistent tiredness.
- Anemia: Often caused by iron deficiency.
- Skin Rash (Dermatitis Herpetiformis): A blistering, itchy skin rash that is one of the hallmark symptoms of celiac disease.
- Mouth Ulcers and Dental Enamel Defects: Recurrent sores in the mouth and enamel defects in teeth.
- Neurological Symptoms: Headaches, peripheral neuropathy (tingling and numbness in the hands and feet), and cognitive impairment.
- Bone or Joint Pain: Arthritis or osteoporosis can occur due to malabsorption of calcium and vitamin D.
- Growth Issues in Children: Delayed growth and puberty.
- Reproductive Issues: Infertility and recurrent miscarriage.
Non-classical symptoms or associated conditions might include liver abnormalities, depression, and anxiety. Many people with celiac disease have no gastrointestinal symptoms at all, which can make diagnosis challenging.
Diagnosis of Celiac Disease
The diagnosis of celiac disease typically involves a combination of blood tests and an endoscopic biopsy of the small intestine:
- Blood Tests: These look for high levels of certain autoantibodies that are common in celiac disease, such as anti-tissue transglutaminase (tTG) and anti-endomysium antibodies.
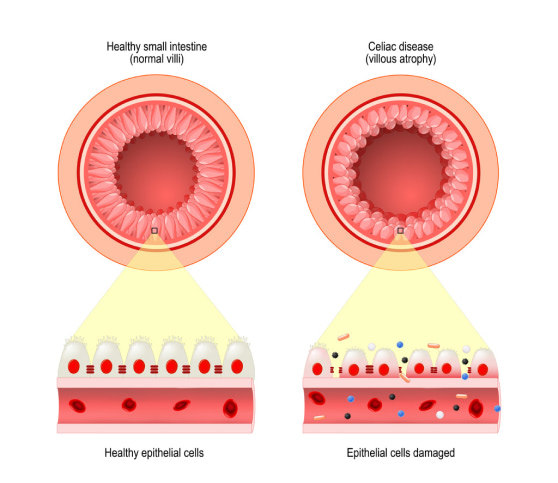
- Endoscopic Biopsy: If blood tests are positive, a biopsy from the small intestine is generally performed to confirm the diagnosis by showing damage to the intestinal villi.
Treatment for Celiac Disease
The only current treatment for celiac disease is a strict, lifelong gluten-free diet. Here’s what this involves:
Avoiding Gluten
- Reading Labels: Carefully read food labels to avoid gluten-containing ingredients. Gluten is often hidden in processed foods, sauces, and even medications.
- Gluten-Free Alternatives: Substitute gluten-containing grains with gluten-free options like rice, corn, quinoa, and certified gluten-free oats.
- Cross-Contamination: Be mindful of cross-contamination with gluten-containing foods, especially when dining out or preparing food at home.
Nutritional Support
- Addressing Nutritional Deficiencies: Supplements may be necessary to correct deficiencies commonly seen in celiac disease, such as iron, calcium, vitamin D, vitamin B12, folate, and zinc.
- Dietitian Consultation: Working with a dietitian experienced in celiac disease can help ensure a balanced and nutritious gluten-free diet.
Managing Associated Conditions
- Regular Follow-Up: Ongoing monitoring with a healthcare provider is important to assess the effectiveness of the gluten-free diet, check for nutritional deficiencies, and screen for associated conditions.
- Screening for Other Autoimmune Disorders: People with celiac disease have a higher risk of other autoimmune disorders, such as type 1 diabetes and thyroid disease, which should be monitored.
Living with Celiac Disease
Living with celiac disease requires continuous vigilance and adjustments to ensure a healthy, fulfilling life. Emotional support plays a crucial role, as adapting to a gluten-free lifestyle can be challenging, particularly when first diagnosed. Building a network of supportive friends and family, as well as perhaps a celiac support group, can provide invaluable assistance and encouragement. Additionally, educating those around you about the seriousness of cross-contamination and the importance of a strict gluten-free diet can help create a safer environment. With the increasing availability of gluten-free products and heightened awareness, managing celiac disease has become more accessible, allowing individuals to maintain a nutritious diet and enjoy a wide variety of foods.
Conclusion
Living with celiac disease requires significant dietary changes and lifestyle adjustments, but with the right support and knowledge, individuals can lead healthy lives without gluten. Anyone experiencing symptoms of celiac disease, especially those with a family history of the disorder, should seek evaluation from a healthcare provider. Early diagnosis and treatment can prevent the complications associated with celiac disease and significantly improve quality of life.
