Hemorrhoids, while rarely talked about, are a common and often discomforting condition experienced by a significant proportion of adults. Characterized by swollen veins in the lower rectum or anus, they can lead to discomfort, embarrassment, and, sometimes, severe pain. Despite their prevalence, many people lack knowledge about their symptoms and the surgical options available for treatment. This article intends to shed light on identifying hemorrhoid symptoms and explore the various surgical interventions that can alleviate this condition.
Introduction to Hemorrhoids: Symptoms and Surgical Treatments
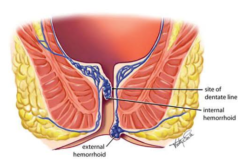
Hemorrhoids, swollen veins in the rectum and anus, are common but can be painful and uncomfortable. Understanding the symptoms and surgical treatment options is essential for those seeking relief. Hemorrhoids can be internal or external, and their cause is generally attributed to excess pressure on the veins in the rectum and anus. This pressure can occur due to various factors, such as chronic constipation, pregnancy, obesity, or prolonged sitting. While some people may experience mild symptoms that do not require treatment, others may need surgical intervention.
Identifying Hemorrhoid Symptoms: Key Indicators to Watch For
Common symptoms of hemorrhoids include rectal bleeding, itching or irritation in the anal region, discomfort or pain, swelling around the anus, and a lump near the anus, which may be sensitive or painful. Recognizing these symptoms is the first step toward getting appropriate treatment. However, these symptoms can also be indicative of other conditions, such as anal fissures or rectal cancer. Therefore, it is essential to consult a doctor for an accurate diagnosis.
When Is Surgery Necessary for Hemorrhoids?
Surgery is considered for hemorrhoids when other treatments, such as lifestyle changes and medications, have not provided relief or when hemorrhoids are particularly large, painful, or prone to bleeding. Additionally, surgery may be recommended if the hemorrhoids are causing complications such as prolapse (when internal hemorrhoids protrude from the anus) or thrombosis (when a blood clot forms in an external hemorrhoid).
Understanding Hemorrhoidectomy: The Surgical Procedure for Hemorrhoid Removal
Hemorrhoidectomy is a surgery to remove excessive hemorrhoidal tissue. This procedure is typically recommended for severe cases of hemorrhoids that have not responded to other treatments. During this surgery, the doctor makes incisions around the hemorrhoid and removes the excess tissue. Recovery can take a few weeks, and some discomfort may be experienced during bowel movements.
Less Invasive Surgical Options: Rubber Band Ligation and Other Procedures
Less invasive procedures like rubber band ligation, sclerotherapy, and infrared coagulation can be effective for treating certain types of hemorrhoids. These procedures typically involve less pain and quicker recovery times than a hemorrhoidectomy. However, they may not be suitable for more severe cases.
Preparing for Hemorrhoid Surgery: What Patients Need to Know
Preparation for hemorrhoid surgery may include a bowel cleanse, fasting, and arranging for recovery time post-surgery. Your doctor will provide specific instructions based on the procedure type. It is essential to follow these instructions closely for a successful surgery and recovery.
Recovery After Hemorrhoid Surgery: Managing Discomfort and Ensuring Healing
Post-surgery recovery can vary depending on the type of procedure performed. Most patients experience some pain and discomfort, which can be managed with pain relief medications and home care strategies. These may include using sitz baths, keeping the anal area clean, and avoiding straining during bowel movements. It is important to follow post-surgery care instructions provided by your doctor for optimal healing.
Potential Risks and Complications of Hemorrhoid Surgery
As with any surgery, hemorrhoid procedures carry some risks, including bleeding, infection, and reactions to anesthesia. Discussing these risks with your healthcare provider is crucial. Additionally, following all pre- and post-surgery instructions can help minimize the chances of complications.
Lifestyle Changes to Prevent Hemorrhoid Recurrence Post-Surgery
After recovering from hemorrhoid surgery, lifestyle changes can help prevent recurrence. These include eating a high-fiber diet, staying hydrated, exercising regularly, and avoiding straining during bowel movements. Additionally, it is essential to address any underlying causes of hemorrhoids, such as chronic constipation or obesity.
Emerging Trends in Hemorrhoid Treatment and Surgery
Advancements in medical technology are continually shaping the treatment and surgical options for hemorrhoids, offering more effective and less invasive methods to manage this condition. These emerging trends include laser treatments, radiofrequency ablation, and stapled hemorrhoidopexy. Discussing these options with your doctor can help determine the best course of treatment for your case.
