What is Colon Cancer?
Colon or colorectal cancer develops in the colon or rectum, parts of the large intestine. It typically begins as small, noncancerous growths called polyps. Over time, some of these polyps may become cancerous and spread into surrounding tissues. Colon cancer is one of the most common cancers worldwide and a leading cause of cancer-related deaths, but it is also highly preventable and treatable when detected early.
Several factors contribute to the development of colon cancer, including lifestyle, environmental exposure, and genetic predisposition. Understanding the role of genetics and undergoing appropriate testing are essential steps in identifying risk and initiating timely interventions.
The Role of Genetics in Colon Cancer
Genetics plays a significant role in the development of colon cancer. While most cases occur sporadically without a family history, approximately 25% are linked to hereditary or familial factors. Genetic mutations passed from parents to offspring can increase an individual's susceptibility to colon cancer.
Hereditary cancer syndromes, such as Lynch syndrome (hereditary nonpolyposis colorectal cancer, or HNPCC) and familial adenomatous polyposis (FAP), are well-documented genetic conditions associated with colon cancer. Lynch syndrome is the most common inherited form of colon cancer caused by mutations in genes responsible for repairing damaged DNA, such as MLH1, MSH2, MSH6, PMS2, and EPCAM. Individuals with Lynch syndrome have a significantly higher risk of developing colon cancer, often at a younger age.
Mutations in the APC gene cause familial adenomatous polyposis and lead to the development of hundreds to thousands of polyps in the colon and rectum during adolescence or early adulthood. Without treatment, nearly all individuals with FAP will develop colon cancer by the age of 40. Other genetic conditions, such as MUTYH-associated polyposis (MAP) and Peutz-Jeghers syndrome, also contribute to colon cancer risk.
Even in the absence of hereditary syndromes, having a first-degree relative (parent, sibling, or child) with colon cancer increases the risk of developing the disease. This familial clustering may result from shared genetic and environmental factors.
Importance of Genetic Testing
Genetic testing can identify mutations associated with an increased risk of colon cancer. For individuals with a family history of the disease or a known hereditary cancer syndrome, genetic testing provides valuable information about their risk. It guides decisions about screening and preventive measures.
Testing typically involves analyzing a blood or saliva sample for specific genetic mutations. Individuals diagnosed with colon cancer at a young age, those with multiple family members affected by the disease, or those with a history of related cancers (such as endometrial or ovarian cancer) may benefit most from genetic testing.
Genetic testing helps identify individuals who carry the mutation and those who do not in families with hereditary cancer syndromes. For carriers, enhanced surveillance and preventive strategies can be implemented. For non-carriers, testing offers reassurance and may reduce the need for intensive screening.
Screening Tests for Colon Cancer
Screening is essential for detecting colon cancer at an early stage or identifying precancerous polyps before they develop into cancer. Several screening methods are available, and the choice depends on individual risk factors, preferences, and accessibility.
Colonoscopy
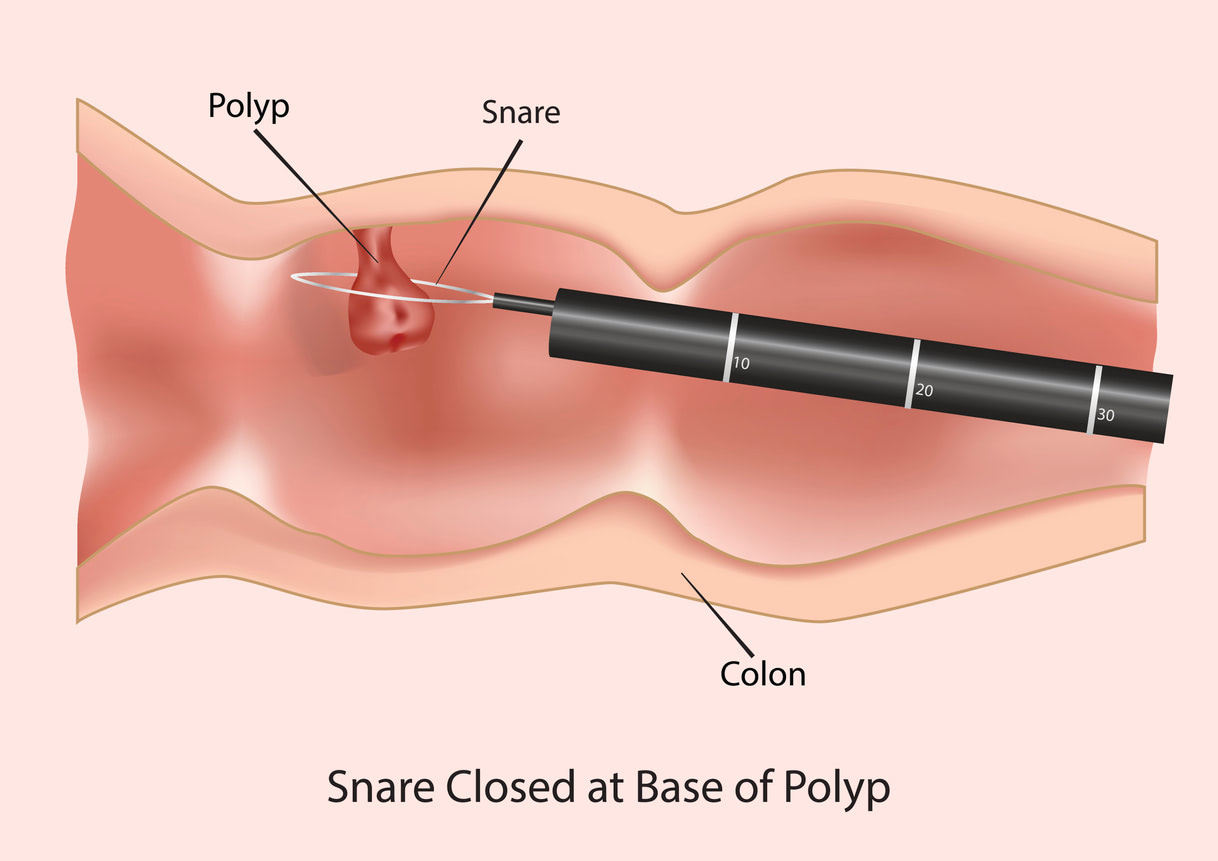
A colonoscopy is the gold standard for colon cancer screening. During the procedure, a flexible tube with a camera is inserted into the rectum to examine the entire colon. Any polyps or abnormal growths can be removed and biopsied during the same procedure. Colonoscopies are recommended every 10 years for individuals at average risk, starting at age 45. Those with a family history or genetic predisposition may need to begin screening earlier and undergo it more frequently.
Stool-Based Tests
Stool-based tests, such as the fecal immunochemical test (FIT) and stool DNA tests, detect blood or abnormal DNA in the stool, which may indicate the presence of polyps or cancer. These non-invasive tests are convenient and can be done at home. However, if the results are positive, a follow-up colonoscopy is required to confirm the findings.
Sigmoidoscopy
A sigmoidoscopy examines only the lower part of the colon and rectum using a flexible tube with a camera. While less comprehensive than a colonoscopy, it is an effective screening tool for identifying abnormalities in the distal colon.
CT Colonography
Also known as a virtual colonoscopy, this test uses CT imaging to create detailed pictures of the colon and rectum. It is less invasive than a traditional colonoscopy but still requires bowel preparation. If abnormalities are detected, a follow-up colonoscopy is needed for further evaluation.
Preventive Measures for Individuals at High Risk
For individuals with a genetic predisposition or a strong family history of colon cancer, preventive strategies go beyond standard screening. These measures may include:
- Increased Surveillance: Individuals with hereditary syndromes often require earlier and more frequent screenings. For example, those with Lynch syndrome may need colonoscopies every 1-2 years starting in their 20s.
- Preventive Surgery: In cases like FAP, prophylactic removal of the colon (colectomy) is often recommended to prevent cancer.
- Lifestyle Modifications: Adopting a healthy lifestyle can reduce overall cancer risk. This includes maintaining a balanced diet rich in fruits, vegetables, and whole grains, engaging in regular physical activity, avoiding smoking, and limiting alcohol intake.
Conclusion
Colon cancer is a serious but preventable disease. Understanding its genetic underpinnings helps individuals and families proactively reduce their risk and detect the disease early. Genetic testing and regular screenings are invaluable tools for identifying high-risk individuals and implementing timely interventions.
For those with a family history of colon cancer or hereditary syndromes like Lynch syndrome or FAP, enhanced surveillance and preventive strategies are essential. Early detection through routine colonoscopies and other tests significantly improves treatment outcomes and survival rates. By combining advanced testing techniques with lifestyle changes, it is possible to reduce the impact of colon cancer and ensure better health outcomes for individuals and future generations.
