Introduction: Understanding Hemorrhoids
Hemorrhoids are swollen veins in the anal or rectal area that can cause discomfort, pain, and bleeding. They are a common condition that can affect people of all ages but are particularly prevalent in individuals with a sedentary lifestyle, chronic constipation, or prolonged straining during bowel movements. While many cases of hemorrhoids are managed through lifestyle changes and non-invasive treatments, some instances require surgical intervention. This article will delve into the causes and symptoms of hemorrhoids and provide a detailed look at both non-surgical and surgical treatment options, helping you make informed decisions about your health. You can visit Mayo Clinic’s Hemorrhoids Overview for more detailed information on hemorrhoids.
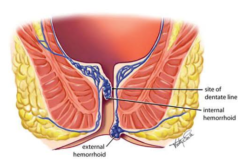
What Are Hemorrhoids?
Hemorrhoids are classified into two main types: internal and external. Internal hemorrhoids form within the rectum and are usually painless, though they can bleed. External hemorrhoids develop under the skin around the anus and tend to be more painful, especially when thrombosed. Both types occur when the veins in the anal region become inflamed or enlarged due to increased pressure, which may result from factors such as prolonged sitting, heavy lifting, chronic constipation, or pregnancy.
The condition is often associated with discomfort during bowel movements. It can sometimes lead to complications like bleeding or, in severe cases, tissue necrosis. Understanding the differences between internal and external hemorrhoids is essential, as it influences both the symptoms experienced and the treatment approach.
Recognizing the Symptoms
The symptoms of hemorrhoids can vary based on their type and severity. Common symptoms include:
- Pain and Discomfort: External hemorrhoids often cause significant pain, especially during or after bowel movements. The pain may be sharp or throbbing.
- Itching and Irritation: The affected area may become itchy or irritated, particularly if hygiene is compromised or the hemorrhoids are aggravated by friction.
- Bleeding: Bright red blood may appear on the toilet paper or in the toilet bowl. While bleeding from hemorrhoids is usually not severe, it can be a sign of significant inflammation.
- Swelling and Lumps: Swollen lumps near the anus, which can be tender to touch, are typical of external hemorrhoids. Internal hemorrhoids may also prolapse, causing a feeling of fullness or a protruding mass.
For many, these symptoms are intermittent, but the pain and discomfort can interfere with daily activities and quality of life during flare-ups.
Non-Surgical Management: First-Line Treatments
In many cases, hemorrhoids can be managed with conservative treatments that focus on reducing inflammation and easing discomfort. Non-surgical strategies include both lifestyle modifications and over-the-counter remedies:
Lifestyle and Dietary Adjustments
A crucial aspect of managing hemorrhoids is making changes to reduce the strain on your anal region. Here are some effective strategies:
- Improve Your Diet: A high-fiber diet that includes fruits, vegetables, and whole grains can help soften stools and promote regular bowel movements. This reduces the need for strain during defecation. Drinking plenty of water is equally essential to maintain proper hydration.
- Avoid Straining: Make a conscious effort to avoid straining during bowel movements. Establishing regular bathroom habits and not delaying the urge to defecate can help reduce the pressure on the hemorrhoidal veins.
- Exercise Regularly: Physical activity, such as walking or light aerobic exercises, improves circulation and can help maintain a healthy digestive system. Regular exercise also aids in weight management, which is beneficial since excess weight increases abdominal pressure.
- Sitz Baths: Soaking in a warm sitz bath for 10 to 15 minutes several times a day can soothe the affected area, help relieve pain, and reduce inflammation.
Over-the-Counter Treatments
Over-the-counter remedies are often used to alleviate the symptoms of hemorrhoids:
- Topical Creams and Ointments: These products often contain ingredients like hydrocortisone or witch hazel, which can reduce inflammation and provide temporary pain relief.
- Pain Relievers: Over-the-counter pain medications, such as acetaminophen or ibuprofen, can help manage pain and reduce swelling.
- Cold Compresses: Applying an ice pack or cold compress to the affected area may help decrease swelling and numb the pain.
While these treatments can provide relief, they are generally considered temporary solutions. More advanced treatments, including surgical options, may be necessary if symptoms persist despite these measures.
When Is Surgery Necessary?
Surgery is typically considered when hemorrhoids do not respond to conservative treatments or if complications arise. Some indications that surgery may be required include:
- Persistent, Severe Pain: When hemorrhoid pain becomes chronic and interferes with daily activities, surgery may be recommended.
- Recurrent Bleeding: Ongoing or heavy bleeding that leads to anemia or significant discomfort can signal the need for surgical intervention.
- Thrombosed Hemorrhoids: When a blood clot forms in an external hemorrhoid, the pain can be excruciating, and surgery may provide rapid relief.
- Prolapsed Hemorrhoids: Internal hemorrhoids that protrude from the anus and do not retract on their own may require surgical removal to alleviate symptoms and prevent further complications.
It’s important to note that surgery is considered a last resort after non-surgical methods have been exhausted. A thorough evaluation by a healthcare provider is essential to determine the appropriate treatment plan based on the severity of the condition.
Pre-Surgical Considerations
Before undergoing surgery for hemorrhoids, several pre-operative steps are typically followed:
- Medical Evaluation: Your healthcare provider will conduct a comprehensive evaluation to assess your overall health, the severity of your hemorrhoids, and any underlying conditions that may affect the procedure.
- Preparation Instructions: Your doctor will provide specific instructions regarding dietary restrictions, medications, and bowel preparation to ensure a clear surgical field.
- Discussion of Options: Different surgical techniques may be available, and your doctor will discuss each option's risks and benefits. This informed consent process is crucial for setting realistic expectations and ensuring you are comfortable with the planned intervention.
The Surgical Procedure: What to Expect
Several surgical procedures can effectively treat hemorrhoids, and the choice of procedure depends on the severity and type of hemorrhoids present. Common surgical interventions include:
- Hemorrhoidectomy: This traditional surgical method involves the complete removal of hemorrhoidal tissue. It is highly effective for severe cases but may involve a more extended recovery period and postoperative discomfort.
- Stapled Hemorrhoidopexy: Also known as stapled hemorrhoid surgery, this procedure involves repositioning the hemorrhoids and reducing blood flow to them. It tends to be less painful and allows for a faster recovery compared to a full hemorrhoidectomy.
- Minimally Invasive Techniques: Procedures such as rubber band ligation, infrared coagulation, and sclerotherapy are less invasive alternatives suitable for more minor or less severe hemorrhoids. These techniques often offer shorter recovery times but might require multiple sessions for optimal results.
You will typically receive anesthesia or sedation during the procedure to ensure comfort. Depending on its complexity and your overall health status, the chosen method will be performed in an outpatient setting or hospital.
Post-Surgery Care and Recovery
After surgery, proper postoperative care is essential for a smooth recovery and to minimize the risk of complications. Key aspects of post-surgery care include:
- Pain Management: Your doctor will prescribe pain medications to help manage postoperative discomfort. It is essential to follow the prescribed dosage and schedule.
- Wound Care: It is vital to keep the surgical area clean and dry. Your doctor will provide specific instructions on how to care for the area to prevent infection.
- Diet and Hydration: A soft, high-fiber diet can aid recovery by reducing strain during bowel movements. Drinking plenty of fluids is equally essential to prevent dehydration and facilitate healing.
- Activity Restrictions: You may need to limit physical activity for a few days or weeks after surgery. Avoiding heavy lifting and prolonged sitting can help reduce pressure on the affected area.
- Follow-Up Appointments: Regular follow-up visits with your healthcare provider are necessary to monitor your progress and address any concerns promptly.
For additional details on postoperative care, you can consult resources provided by the American Gastroenterological Association.
Long-Term Management and Prevention
Even after successful surgery, long-term management of hemorrhoids is essential to prevent recurrence. Some strategies include:
- Maintaining a High-Fiber Diet: Consistently consuming a fiber-rich diet helps ensure regular bowel movements and reduces the risk of constipation, a major contributor to hemorrhoid development.
- Staying Hydrated: Adequate water intake supports digestive health and aids in the prevention of straining during bowel movements.
- Regular Physical Activity: Moderate exercise improves circulation and helps maintain a healthy weight, both of which are important for reducing the risk of hemorrhoids.
- Healthy Bowel Habits: Avoid straining during bowel movements, and establish a regular schedule to reduce the pressure on the anal veins.
- Monitoring Symptoms: Stay alert to recurring symptoms such as pain, bleeding, or discomfort, and seek medical advice promptly if symptoms return.
Integrating these preventive measures into your daily routine can reduce the likelihood of future hemorrhoid flare-ups and maintain long-term digestive health.
Psychological and Social Considerations
The experience of dealing with hemorrhoids—especially when symptoms are severe enough to require surgery—can be both physically and emotionally taxing. Patients may experience anxiety, embarrassment, or stress related to their condition. Addressing these psychological aspects is an integral part of the overall treatment. Counseling, support groups, or speaking with a healthcare provider about your concerns can provide reassurance and help you cope with the challenges of recovery and long-term management.
Conclusion: Empowering Your Path to Relief
Hemorrhoids can significantly impact your quality of life. Still, with the right strategies, both non-surgical and surgical treatments offer effective relief. By understanding the causes and symptoms, you can take proactive steps to manage the condition through dietary modifications, lifestyle adjustments, and, when necessary, surgical intervention. Proper preparation, a carefully executed surgical procedure, and diligent postoperative care contribute to a successful outcome.
Empower yourself by staying informed and working closely with your healthcare team. By committing to preventive measures and healthy lifestyle habits, you can minimize the recurrence of hemorrhoids and enjoy lasting relief. Remember, your journey to better digestive health begins with informed choices and proactive management—small, consistent steps that lead to a brighter, more comfortable future.
