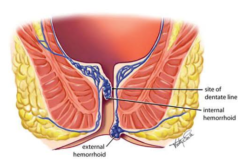
Hemorrhoids, also known as piles, are swollen veins in the anus and lower rectum, similar to varicose veins. They can develop inside the rectum (internal hemorrhoids) or under the skin around the anus (external hemorrhoids). While they are common and not usually life-threatening, hemorrhoids can cause significant discomfort and impact daily activities. Recognizing the symptoms and understanding treatment options, including when surgery is warranted, is important for effective management.
Symptoms of Hemorrhoids
The symptoms of hemorrhoids vary depending on their location and whether they cause complications like thrombosis or prolapse:
- Internal Hemorrhoids may not be visible or cause discomfort initially. However, straining or irritation during bowel movements can cause painless bleeding, typically noticeable as bright red blood on toilet paper or in the toilet bowl. Advanced internal hemorrhoids may prolapse, meaning they stretch and bulge outside the anal sphincter, causing potential pain and irritation.
- External Hemorrhoids are often felt as a lump near the anus and can cause itching, discomfort, and pain, especially when sitting. If an external hemorrhoid becomes thrombosed (develops a blood clot), it can lead to severe pain, inflammation, and a hard lump near the anus.
When Surgery Becomes Necessary
While many hemorrhoids can be managed with home remedies and over-the-counter treatments, certain situations may necessitate surgical intervention:
- Persistent Symptoms: If conservative measures such as dietary changes, sitz baths, and topical treatments fail to alleviate symptoms, surgery may be considered to provide relief.
- Large Hemorrhoids: Large internal or external hemorrhoids that cause significant discomfort or bleeding may require surgical removal.
- Thrombosed External Hemorrhoids: If an external hemorrhoid develops a clot within 72 hours, excision under local anesthesia can provide immediate relief.
- Prolapsed Internal Hemorrhoids: Surgery may be needed for internal hemorrhoids that prolapse and cannot be manually reduced or those that repeatedly prolapse despite conservative treatment.
Surgical Treatment Options
Several surgical procedures are available for treating hemorrhoids, depending on the type and severity:
- Hemorrhoidectomy: This procedure involves the complete removal of the hemorrhoid. Hemorrhoidectomy is considered the most effective treatment for severe or recurrent hemorrhoids but requires a longer recovery period and may be associated with more postoperative pain.
- Stapled Hemorrhoidopexy: Also known as a stapled hemorrhoidectomy, this procedure involves resecting a band of tissue above the hemorrhoid to cut off its blood supply, causing it to shrink. This technique is less painful than a traditional hemorrhoidectomy and has a shorter recovery time, but it may not be suitable for all types of hemorrhoids.
- Rubber Band Ligation: A minimally invasive procedure where a rubber band is placed around the base of an internal hemorrhoid to cut off its blood supply, causing it to wither and fall off within a week. This procedure is effective for bleeding or prolapsing internal hemorrhoids not responsive to conservative treatment.
- Infrared Coagulation: A less invasive treatment that uses infrared light to cause scar tissue, which cuts off the blood supply to the hemorrhoid, causing it to shrink. This method is typically used for smaller hemorrhoids.
Postoperative Care and Recovery
Postoperative care and recovery are crucial aspects of the treatment process for hemorrhoid surgery. Following surgery, patients may experience discomfort, including pain and swelling in the anal area, which can generally be managed with pain relief medications and ice packs. Doctors usually recommend a diet rich in fiber and plenty of fluids to soften stools and prevent constipation, a key factor in avoiding strain during bowel movements. Additionally, sitz baths, or sitting in warm water for 10 to 15 minutes several times a day, can help soothe the area and promote healing. While recovery times vary depending on the type of surgery performed, most patients can resume normal activities within a few weeks, with some precautions to prevent recurrence.
Preventing Hemorrhoid Recurrence
Preventing the recurrence of hemorrhoids involves implementing lifestyle and dietary changes aimed at reducing strain during bowel movements and preventing constipation. It is recommended to include high-fiber foods in your diet, such as fruits, vegetables, and whole grains, to facilitate easier bowel movements and to drink ample fluids to stay hydrated. Regular exercise can also help by improving digestion and reducing the pressure on the veins in your lower rectum and anus, often caused by sitting for prolonged periods. Additionally, avoiding prolonged sitting on the toilet and refraining from straining during bowel movements can significantly reduce the risk of developing hemorrhoids again. Adopting these habits not only aids in recovery after hemorrhoid treatment but also serves as a proactive approach to maintaining rectal health and preventing future episodes.
Conclusion
Hemorrhoids can range from a minor nuisance to a significant source of discomfort. While many cases can be managed with non-surgical methods, surgery becomes an option when these treatments fail to provide relief or in the case of severe hemorrhoids. Understanding the symptoms and treatment options available, including surgical interventions, is key to effectively managing this common condition. Consulting with a healthcare provider is essential for determining the most appropriate treatment based on individual needs and the severity of symptoms.
