What is IBS?
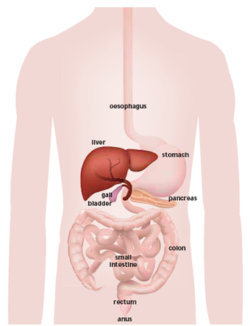
Irritable bowel syndrome (IBS) is a common chronic condition that affects the large intestine, causing symptoms such as abdominal pain, bloating, gas, diarrhea, and constipation. While IBS does not cause permanent damage to the digestive tract or lead to severe diseases like cancer, it can significantly impact a person's quality of life. The exact cause of IBS is not fully understood. Still, it is believed to involve a combination of factors such as abnormal muscle contractions in the intestine, heightened sensitivity to digestion, gut-brain interaction problems, and changes in gut microbiota.
IBS is classified into subtypes based on the predominant symptoms: IBS with diarrhea (IBS-D), IBS with constipation (IBS-C), and IBS with mixed symptoms (IBS-M), where individuals alternate between diarrhea and constipation. Managing IBS requires a multifaceted approach tailored to an individual's specific symptoms and triggers.
Non-Medication Treatments for IBS
Treatment for IBS often begins with lifestyle and dietary changes, which can significantly alleviate symptoms for many people. Identifying and avoiding trigger foods is a cornerstone of IBS management. Common triggers include fatty foods, spicy dishes, caffeine, alcohol, and artificial sweeteners. A dietitian may recommend keeping a food diary to identify specific triggers and help patients develop a personalized eating plan.
One of the most effective dietary strategies for IBS is the low FODMAP diet, which involves reducing foods high in fermentable oligosaccharides, disaccharides, monosaccharides, and polyols. These carbohydrates can be difficult to digest and may exacerbate IBS symptoms. Examples of high-FODMAP foods include onions, garlic, beans, and certain fruits like apples and cherries. The diet typically involves an elimination phase and gradually reintroducing foods to determine tolerance levels.
Stress management is another critical aspect of IBS treatment, as stress is known to worsen symptoms in many individuals. Techniques such as mindfulness meditation, yoga, or cognitive-behavioral therapy (CBT) can help reduce stress and improve gut health by addressing the gut-brain connection. Regular physical activity is also beneficial, promoting healthy digestion and reducing stress-related symptoms.
Medications for IBS
For individuals whose symptoms persist despite lifestyle and dietary changes, medications may be necessary to manage IBS more effectively. The choice of medication depends on the subtype of IBS and the predominant symptoms.
Antispasmodics
Antispasmodic medications, such as hyoscyamine or dicyclomine, are commonly used to relieve abdominal pain and cramping by relaxing the intestine muscles. These medications are particularly effective for individuals who experience significant discomfort due to intestinal spasms. They are typically taken as needed, often before meals, to prevent symptoms.
Laxatives for IBS-C
For those with IBS-C, laxatives can help alleviate constipation. Over-the-counter options like polyethylene glycol (PEG) work by drawing water into the stool, making it easier to pass. Prescription medications such as lubiprostone or linaclotide may also increase intestinal fluid secretion and promote regular bowel movements. These medications are specifically approved for IBS-C and are generally well-tolerated. However, they may cause mild side effects like diarrhea.
Antidiarrheal Medications for IBS-D
For individuals with IBS-D, antidiarrheal medications such as loperamide can help reduce the frequency and urgency of bowel movements. While loperamide does not address abdominal pain, it can significantly improve the quality of life for those struggling with diarrhea. Another option for IBS-D is eluxadoline, a prescription medication that slows intestinal movement while reducing pain.
Fiber Supplements
Fiber supplements, such as psyllium, can benefit individuals with IBS-C and IBS-D by regulating bowel movements. Soluble fiber helps soften stools in constipation while firming stools in diarrhea. However, some types of fiber, like insoluble fiber found in wheat bran, may worsen bloating and gas, so choosing the right type of supplement based on individual symptoms is essential.
Antidepressants
Low doses of antidepressants are sometimes prescribed for IBS, not because the condition is psychological but because these medications affect how the brain and gut communicate. Tricyclic antidepressants (TCAs), such as amitriptyline, are often used for IBS-D, as they slow intestinal motility and relieve pain. For IBS-C, selective serotonin reuptake inhibitors (SSRIs), like fluoxetine, may help speed up intestinal transit. Antidepressants also reduce visceral hypersensitivity, making the gut less sensitive to pain signals.
Antibiotics
For certain individuals, particularly those with bacterial overgrowth in the small intestine, antibiotics like rifaximin can help reduce symptoms of IBS-D. This treatment targets gut bacteria that may contribute to bloating, gas, and diarrhea. Rifaximin is typically used for short-term relief and is effective for some patients with persistent symptoms.
Probiotics
Beneficial bacteria, such as probiotics, may help improve gut health and reduce IBS symptoms by balancing the gut microbiota. Specific strains, such as Bifidobacterium and Lactobacillus, have been shown to reduce bloating, gas, and abdominal pain. While not all probiotics are equally effective, they can be a helpful addition to a comprehensive treatment plan.
Managing IBS Long Term
Living with IBS requires a long-term management plan that may involve a combination of treatments. Regular follow-ups with a healthcare provider are essential to monitor symptoms, adjust treatments, and address new concerns. It is also important for individuals with IBS to remain adaptable, as triggers and symptoms may change over time.
Emotional support and education are critical for helping patients cope with IBS. Many people find support groups or therapy helpful for managing the psychological impact of living with a chronic condition. Understanding that IBS does not cause permanent damage or life-threatening complications can provide reassurance and reduce anxiety about the condition.
Conclusion
IBS is a complex condition that requires a personalized approach to treatment. While lifestyle changes and dietary adjustments often provide relief, medications can be a valuable tool for managing persistent or severe symptoms. By working closely with healthcare providers, individuals with IBS can find the right combination of treatments to improve their quality of life and reduce the impact of this chronic condition. The outlook for managing IBS continues to improve with continued research and advancements in treatment options.
