Introduction: Understanding GERD
Gastroesophageal reflux disease (GERD) is a chronic condition in which stomach acid frequently flows back into the esophagus, leading to discomfort and potential complications over time. This backflow, often experienced as heartburn, is more than an occasional inconvenience—it can significantly affect quality of life if left unmanaged. Understanding the causes of GERD and taking proactive steps to prevent its progression are critical components of long-term digestive health. This article delves into the factors contributing to GERD. It outlines effective prevention strategies to help you maintain a healthier lifestyle. For an in-depth overview of GERD, visit Mayo Clinic’s GERD Information.
What Causes GERD?
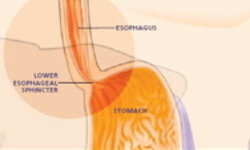
GERD develops when the lower esophageal sphincter (LES)—a ring of muscle at the junction between the esophagus and the stomach—fails to close properly after a meal. This malfunction allows acidic stomach contents to flow back into the esophagus, causing irritation and inflammation. While the underlying mechanism is straightforward, combining factors can weaken the LES or increase stomach acid production, promoting reflux.
One significant factor is diet. Consuming large or fatty meals, spicy foods, chocolate, and caffeinated or carbonated beverages can relax the LES, making reflux more likely. Overeating increases stomach pressure, further straining the LES and encouraging acid to escape upward. In addition to these dietary habits, lifestyle factors such as smoking and alcohol consumption also play a critical role. Smoking weakens the LES and reduces saliva production, which usually helps neutralize stomach acid. Alcohol, on the other hand, can irritate the esophageal lining and disrupt normal digestive processes.
Hormonal influences are another contributor. During pregnancy, for example, increased progesterone levels relax the LES. At the same time, the growing uterus exerts additional pressure on the stomach, leading to an elevated risk of acid reflux. Beyond these common causes, obesity is a significant risk factor. Excess body weight, particularly around the abdomen, increases intra-abdominal pressure, making it more difficult for the LES to function correctly and effectively prevent acid backflow.
Underlying Mechanisms and Risk Factors
Understanding the mechanisms behind GERD involves examining both anatomical and physiological factors. The LES acts as a barrier between the stomach and the esophagus. When it weakens or relaxes inappropriately, it allows the reflux of gastric contents. This reflux can cause chronic inflammation, leading to complications such as esophagitis, Barrett's esophagus, or even an increased risk of esophageal cancer if left untreated.
Several risk factors compound the likelihood of developing GERD. Along with dietary choices and lifestyle habits, genetic predispositions may also influence the integrity of the LES and the overall susceptibility to acid reflux. Moreover, conditions such as hiatal hernia—where part of the stomach pushes into the chest cavity through the diaphragm—further disrupt the normal functioning of the LES, contributing to GERD symptoms.
The combination of these factors creates an environment in which GERD can persist and worsen over time. The interplay between an overactive stomach, a weakened barrier, and external influences ultimately determines the severity and frequency of reflux episodes.
Prevention Strategies: Proactive Steps to Reduce GERD Risk
Prevention is a key aspect of managing GERD, and several lifestyle and dietary modifications can significantly reduce the risk of acid reflux. One of the most effective strategies is to focus on a balanced, healthy diet that minimizes trigger foods. This involves avoiding large meals, reducing the intake of high-fat and spicy foods, and limiting caffeine and alcohol consumption. Eating smaller, more frequent meals can help reduce stomach pressure and lessen the strain on the LES.
Maintaining a healthy weight is also critical. Excess weight increases abdominal pressure, making reflux more likely. Regular exercise not only supports weight management but also improves overall digestive function. Even moderate activities like walking or yoga can help stimulate digestion and lower stress levels, which is essential for preventing GERD.
Another cornerstone of GERD prevention is lifestyle modification. Quitting smoking is one of the most impactful changes you can make, as it directly strengthens the LES and enhances the body’s natural ability to neutralize stomach acid. Additionally, managing stress through techniques such as mindfulness meditation, deep breathing exercises, or counseling can positively affect digestive health. Stress can exacerbate GERD symptoms by increasing acid production and affecting gut motility, so incorporating stress-reduction strategies into your daily routine is essential.
You may also refer to resources provided by the American Gastroenterological Association for a deeper understanding of effective prevention measures.
The Role of Diet in GERD Prevention
Dietary modifications are at the forefront of GERD prevention. A well-planned diet focusing on whole, nutrient-rich foods can make a significant difference in managing reflux symptoms. Emphasize foods low in fat and easy to digest, such as lean proteins, whole grains, fruits, and vegetables. Fiber is particularly important as it helps regulate digestion and can prevent overeating, a known trigger for GERD.
Conversely, identifying and eliminating trigger foods is essential. Many individuals with GERD find that certain foods aggravate their symptoms. Keeping a food diary can help you track what you eat and how it affects your reflux. This personalized approach allows you to pinpoint specific foods that may be problematic and adjust your diet accordingly. Eating slowly and chewing thoroughly is also beneficial, as this improves digestion and reduces the likelihood of overeating.
Hydration is another key factor in a GERD-friendly diet. Drinking daily water helps dilute stomach acid and promotes overall digestive health. However, avoiding drinking large amounts of water during meals is advisable, as this can increase stomach volume and potentially contribute to reflux.
Lifestyle Modifications for GERD Prevention
In addition to dietary adjustments, various lifestyle modifications can play a significant role in preventing GERD. Regular physical activity is one of the most effective ways to support digestive health. Exercise helps to improve gastrointestinal motility and reduces the likelihood of constipation, which can exacerbate reflux symptoms. Whether it’s a daily walk, a yoga session, or another form of moderate exercise, staying active is essential.
Stress management is equally important. Chronic stress can profoundly impact digestion by increasing stomach acid production and disrupting normal gut function. Integrating stress-relief practices into your routine—such as meditation, deep breathing exercises, or even hobbies that help you relax—can mitigate the impact of stress on your digestive system.
Moreover, simple habits like elevating the head of your bed can contribute to GERD prevention. Sleeping with your head slightly elevated allows gravity to help keep stomach acid from flowing back into the esophagus during the night. Avoiding lying down immediately after meals is another effective strategy; waiting at least two to three hours is generally recommended before reclining.
Monitoring and Regular Check-Ups
Even with preventive measures, monitoring your symptoms and maintaining regular check-ups with your healthcare provider is essential. Early detection of worsening symptoms can allow for timely adjustments in your prevention strategy. Regular visits to your doctor can help ensure that your lifestyle and dietary modifications are practical and provide an opportunity to discuss any concerns that may arise.
Tracking your progress through a symptom diary can also be a valuable tool. You can identify trends and make further adjustments by noting changes in your symptoms, dietary habits, and lifestyle practices. This proactive approach not only aids in managing GERD but also helps in the early detection of any potential complications.
Psychological and Emotional Considerations
Living with GERD can sometimes take an emotional toll, especially when symptoms interfere with daily activities or cause discomfort. It is essential to recognize that managing GERD is not just about physical changes but also involves addressing emotional and psychological well-being. Stress and anxiety can exacerbate reflux symptoms, creating a cycle that is difficult to break. Seeking support—whether through professional counseling, support groups, or simply sharing your experiences with friends and family—can provide relief and help you cope with the challenges of the condition.
Conclusion: Taking Control of Your Digestive Health
GERD is a multifactorial condition influenced by dietary habits, lifestyle choices, and physiological factors. Understanding the underlying causes and adopting proactive prevention strategies can significantly reduce the risk of acid reflux and improve your overall digestive health. Emphasizing a balanced diet, maintaining a healthy weight, engaging in regular physical activity, and managing stress are all essential components of a comprehensive GERD prevention plan.
Empower yourself with knowledge and make informed choices about your lifestyle. Regular monitoring and communication with your healthcare provider will help you stay on track and adjust your strategies as needed. With dedication and proactive care, you can take control of your digestive health and reduce the impact of GERD on your daily life.
Remember, small, consistent changes can lead to significant improvements over time. Stay committed to your prevention plan and enjoy the benefits of a healthier, more comfortable life.
